

Included are selected materials developed by expert NRHI member faculty and based on the priority needs of the Transforming Clinical Practice Initiative Community
The bundle includes easily accessible learning modules with short videos and key takeaways around topics related to sustaining and ongoing efforts on QI initiatives and programming.
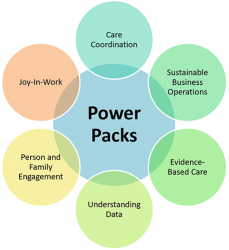
Each Power Pack solves a specific challenge that a practice might face as it begins the process of clinical practice transformation. They demonstrate specific pathways to resolve healthcare delivery challenges.
Primary and specialty care providers face many challenges as they navigate the complex landscape to transition their practice from a model focused on volume, to value.
~~~


~~~
Depression screening tutorial produced by CMS (Published on Sep 2, 2010)
The systematic inclusion of resident voice through specific direct interviews represents an enormous advance in the new Minimum Data Set 3.0 (MDS 3.0). The Video on Interviewing Vulnerable Elders (VIVE) demonstrates best practice approaches for implementing the new MDS interviews for cognition, mood, preferences and pain. Specific video sections address the reason interviews have been added, techniques to improve communication with older, frail populations, and demonstration of each interview being conducted. Using real life nurses interacting in scenarios based on actual situations, VIVE helps to build understanding and ease implementation of MDS 3.0 for nursing home staff members. The goal of VIVE, funded by the Picker Institute and developed by the UCLA/Jewish Home Borun Center, is to help staff members build the confidence and skills they need to interview their residents both for MDS 3.0 and for other clinical evaluations. Watch video.
On June 22nd, 2017 MHQP hosted a conversation in which we described our patient experience surveying program and how to use the results to improve quality. We were joined by leaders at two provider organizations that have real world experience in working with their staffs to use PES results to provide more patient-centered care. Each has seen its scores and its patients’ experience improve dramatically over time.
Suzanne Countie from Lowell General PHO talked about how important it is to make a connection with the patient, and that it all starts with empathy. Check out this Cleveland Clinic Video: Empathy: The Human Connection to Patient Care. Dr. Hartmann talked about as pecific program developed for asthma that resulted in his practice having the lowest emergency room visits for children with asthma among all the practices in the Pediatric Physicians’ Organization at Children’s (PPOC).
Check out the recording from our live event here: NRHI SAN: How to Help Clinicians Take Action with their PES Results. Additional resources, including the slide deck from the event, and a Q and A document coming soon, can be in the Resources section in this group.
Survey templates available from AHRQ CAHPS that you might want to use include:
Key takeaways from the presentation included:

The BOOSTing (Better Outcomes by Optimizing Safe Transitions) Care Transitions implementation toolkit provides a wealth of materials to help you optimize the discharge process at your institution.
The tools and approach are based on principles of quality improvement (QI), evidence-based medicine, as well as personal and institutional experiences.
Watch NRHI’s vlog on how Choosing Wisely can help patients and doctors avoid unnecessary and costly care. This is one way to advance healthcare affordability.
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |